Chronic pain is more than an occasional ache. It's pain that persists for three months or longer, sometimes even after an injury has healed. Unlike short-term pain, chronic pain can affect sleep, mood, ability to work, and overall quality of life.
Patients often describe it as a dull ache, sharp stabbing, burning, or tingling sensation. For some, it's constant. For others, it comes and goes unpredictably. Understanding the source of pain is key to finding relief.
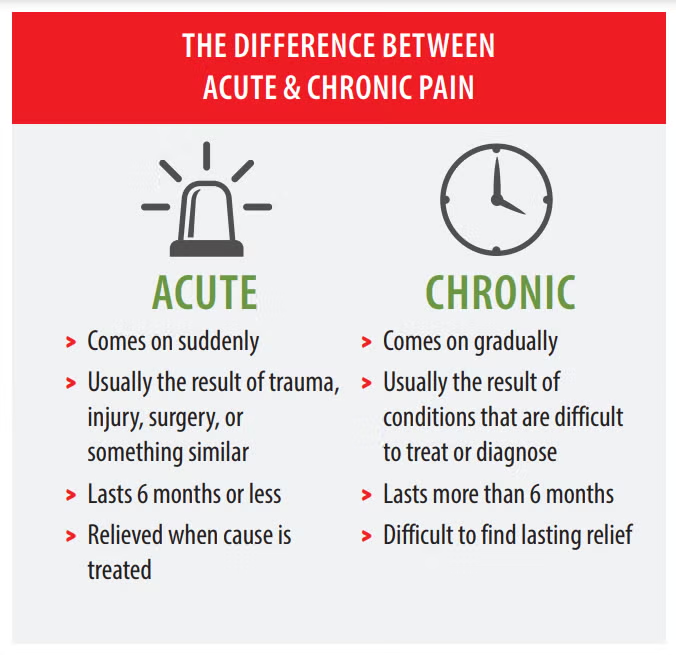
Acute pain serves a clear purpose. It's the body's alarm system alerting you to injury or illness. When you sprain an ankle or recover from surgery, acute pain gradually fades as healing occurs. This type of pain is temporary and directly linked to tissue damage.
Chronic pain works differently. It can continue long after tissues have healed, sometimes developing into a condition of its own. The nervous system can become oversensitive, sending pain signals even when there's no ongoing injury. This isn't psychological or imaginary. It represents real changes in how nerves process and transmit signals.
Some patients develop chronic pain after a clear injury or surgery. Others notice it developing gradually over months or years. In some cases, there's no obvious triggering event at all.
There isn't always a single reason why chronic pain develops. Often, it's a combination of factors including injuries, medical conditions, and lifestyle influences.
1. Back and Neck Issues
Problems in the spine, such as herniated discs, degenerative changes, or muscle strain, are common culprits. Poor posture, repetitive work motions, or prolonged sitting can worsen these conditions over time. The spine supports the entire body, so even minor misalignments or weaknesses can create significant discomfort.
2. Joint Pain
Arthritis, bursitis, tendonitis, or injuries can lead to persistent joint discomfort. Even small, repeated stresses on knees, hips, shoulders, or hands can trigger long-term pain that affects mobility and daily function. Athletes, manual laborers, and people who perform repetitive motions at work are particularly vulnerable.
3. Nerve-Related Pain
Conditions like sciatica or peripheral neuropathy create sharp, radiating, or tingling sensations in the arms or legs. Nerve pain is often unpredictable and can interfere with sleep, movement, and daily routines. Diabetes, injuries, and compression from spinal issues are common causes of nerve damage.
4. Previous Injuries or Surgeries
Sometimes pain persists after an injury has healed or surgery has been completed. Scar tissue, altered movement patterns, or changes in how the nervous system processes signals can all contribute to ongoing discomfort months or years later.
5. Medical Conditions
Fibromyalgia, autoimmune disorders, and other systemic conditions can cause widespread chronic pain. These conditions often involve inflammation, immune system dysfunction, or nervous system changes that make the body more sensitive to pain signals.
6. Lifestyle Factors
Stress, lack of exercise, poor sleep, and repetitive strain can make pain worse. Sometimes the body's response to stress and fatigue amplifies pain signals, keeping discomfort ongoing even after an injury heals.
Not all pain needs immediate medical attention, but certain signs indicate it's time to see a specialist:
Addressing these issues early can prevent complications and improve outcomes. Many patients wait months or even years before seeking specialized care, but earlier intervention often leads to better results.
Many patients assume surgery or opioid medications are the only options. In reality, there are safe, effective alternatives that often provide long-term relief.
Physical Therapy
Guided exercises help strengthen muscles, improve posture, and reduce pressure on painful areas. Physical therapy also teaches techniques to use at home to prevent flare-ups and maintain progress. A good physical therapist creates an individualized program based on specific needs and limitations.
Pain Management Injections
Targeted injections, such as nerve blocks or joint injections, can reduce inflammation and relieve pain. These procedures often allow patients to participate more fully in physical therapy and resume normal activities. Injections aren't a permanent fix for everyone, but they can provide significant relief and break the pain cycle.
Chiropractic Care and Acupuncture
These approaches can help restore joint mobility, reduce muscle tension, and improve overall comfort. Many patients find relief through these complementary treatments as part of a broader pain management plan.
Non-Opioid Medications
Anti-inflammatories, topical creams, and nerve-modulating medications can safely manage pain without the risks of opioids. These options work differently than pain pills, often targeting the source of discomfort rather than just masking symptoms.
Lifestyle Adjustments
Regular low-impact exercise, ergonomic workstations, proper sleep, and stress management strategies such as mindfulness or yoga can all reduce pain severity. Small changes in daily habits often make a significant difference in pain levels. Weight management, smoking cessation, and proper nutrition also play important roles.
Cognitive Behavioral Therapy
This type of therapy helps change how patients think about and respond to pain. It doesn't suggest that pain is imaginary, but rather teaches techniques to reduce the emotional distress and physical tension that can worsen pain.
Occupational Therapy
Learning new ways to perform daily tasks can reduce strain and prevent pain flare-ups. Occupational therapists can recommend adaptive equipment, teach energy conservation techniques, and help patients maintain independence despite chronic pain.
Effective chronic pain management rarely relies on a single treatment. Most patients benefit from a combination of approaches tailored to their specific situation.
A comprehensive evaluation is the starting point. This includes medical history, physical examination, and sometimes imaging studies or diagnostic tests. Understanding what's causing the pain helps determine which treatments are most likely to help.
Treatment typically begins with conservative approaches. Physical therapy, medications, and lifestyle modifications form the foundation. If these aren't sufficient, interventional procedures or more specialized treatments may be added.
Progress takes time. Most patients don't see dramatic improvement overnight. Instead, relief builds gradually over weeks or months. Patience and consistency with treatment recommendations are essential for success.
Will the pain ever go away?
Chronic pain can sometimes persist indefinitely, but with proper management, most patients see meaningful improvement. The goal is to restore function, reduce discomfort, and improve quality of life rather than chasing complete elimination of all sensation.
Which treatment is right for me?
Treatment depends on the source of pain, health history, and lifestyle. A pain specialist will evaluate the condition and create a personalized plan that may combine several approaches for best results.
Are non-surgical treatments effective?
Yes. Many patients experience significant relief through physical therapy, injections, lifestyle adjustments, and non-opioid medications. Surgery is typically considered only when other options haven't provided adequate relief.
How long does treatment take?
This varies by individual and condition. Some patients notice improvement within weeks, while others require several months of consistent treatment. Chronic pain that has been present for years often takes longer to improve than more recent pain.
Will I need treatment forever?
Some patients achieve lasting relief and can stop or reduce treatment over time. Others manage chronic pain as an ongoing condition, similar to other chronic health issues. The goal is to maximize function and comfort with the least invasive, most sustainable approach possible.
If pain has lasted for months, affects daily life, or hasn't improved with home care, it's time to seek professional help. A pain specialist can identify the underlying cause of pain, recommend the most effective treatments, and provide ongoing support and adjustments as needed.
Pain specialists have advanced training in diagnosing and treating complex pain conditions. They stay current with the latest research and treatment options, offering approaches that may not be available through general practitioners.
Chronic pain doesn't have to control your life. With the right guidance, it's possible to regain comfort, mobility, and the ability to enjoy everyday activities again.
Take the First Step
Don't wait for pain to worsen. Contact Integrative Sports and Spine today to schedule a consultation and learn how non-surgical, personalized treatment can help you feel better.